P.G.L. of Tyrone and Fermanagh
The Prostate Gland
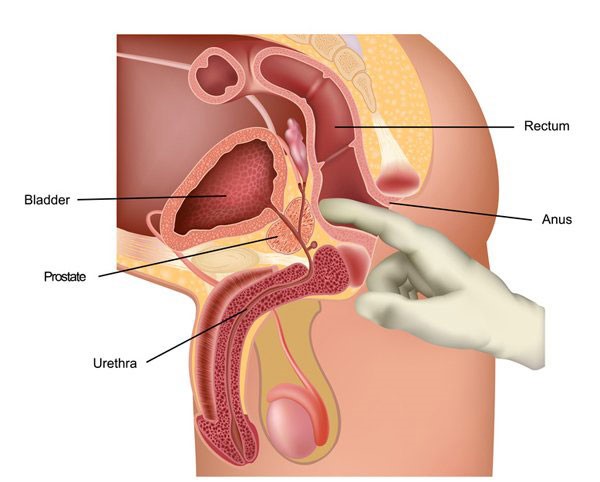
The Prostate gland specific to males only, located in the pelvis between the bladder and rectum. It is about the shape and size of a walnut or satsuma and gets bigger as you get older. It surrounds the urethra which is the tube men urinate and ejaculate through. Its main function is to assist in the making of semen, the fluid that transports the sperm.
The prostate can be affected by three conditions that may cause problems for men as they get older.
1. An enlarged prostate
This is the most common problem; common in men over 50; this may be called Benign Prostatic Hyperplasia (BPH) or Benign Prostatic Enlargement (BPE). BPH is not cancerous and there are various avenues of treatment; as the prostate enlarges with age it presses on the urethra and can slow down or stop the passage or urine. The treatment you are given will depend on how severe your symptoms are, usually either drug treatment or surgery.
2. Prostatitis
This can be caused by infection or inflammation of the gland. Can occur at any age but is more common between 30 and 50 years. Symptoms - These are wide ranging and common to other conditions. These may include urinary problems, burning when you pass urine, fever, in severe cases may cause aching in between your testicles and back passage, pain in the groin, lower back or your stomach area, pain in the inner thigh area. There are different types of prostatitis and therefore are treated in different ways.
3. Prostate Cancer - The facts
It's the most common cancer in men in the UK with over 40,000 new cases diagnosed each year. The risk of developing prostate cancer increases with age. About 10% are diagnosed in their 50's. Most men are diagnosed in their 70's and by the age of 80 most men will have some prostate cancer cells. Only a small number (about 4%) of all men will die from prostate cancer.
Note:
- You can have prostate cancer at a much younger age.
- Not all prostate cancers present with distinct symptoms.
- The symptoms of the three prostate conditions share some common symptoms.
- Needing to urinate more frequently, especially at night - (Nocturia)
- Slow to start to pass urine (Hesitancy)
- A weak flow when passing urine (Poor Stream)
- Straining or taking a long time to finish.
- A feeling that you're not emptying your bladder fully
- Sometimes leaking before you get there.
- Need to push to urinate occasionally leaking before you get to the toilet.
- Dribbling urine after you finish (Post Micturition Dribble)
Other symptoms can occur less frequently:
Pain when urinating, pain when ejaculating, blood in the urine or semen; problems getting or keeping an erection though most men with this problem do not have prostate cancer. Urinary problems are common in older men but something can always be done to try cure or manage them.
For some men the first symptom of Prostate Cancer might be new pain in the back, hips or pelvis. Symptoms that the cancer may have spread include bone and back pain, loss of appetite, pain in the testicles or unexplained weight loss.
What is Prostate Cancer?
Normally the growth of all cells is carefully controlled. As cells die they are replaced in set regulated fashion. When cancer develops the cells multiply in an uncontrolled fashion, if this happens in the prostate, prostate cancer can develop. In most cases this is a slow growing cancer and may stay undiagnosed throughout a man's lifetime and may never cause symptoms or problems, however some men will have cancer that needs treatment to prevent and delay it spreading outside the gland.
Risk Factor:
- The risk increases with age, most are over 50 however younger men can be affected.
- Body weight - being overweight or obese increases your risk factors of getting, aggressive (more likely to spread) or advanced cancer that has spread outside the prostate.
- Family History - You are 2½ times more likely to get it if you father or brother has been diagnosed. The risk is even greater if they were under 60 when they were diagnosed or if more than one close relative was diagnosed.
Having a close female relative that has had breast cancer also increases your risk. There is currently no genetic test for prostate cancer.
Ethnicity - African Caribbean are three times more likely to develop prostate cancer than white men. Asian men have a lower risk.
Diet
- Reducing the amount of red meat and processed meat products in your diet.
- Eating a wide range of fruits and vegetables.
- Eating fewer dairy products. There is evidence that a diet high in calcium is linked to an increased risk.
- Exercising regularly.
Research has shown that the risk of prostate cancer appears to be lower in men who eat food containing lycopene found in cooked tomatoes and other red fruit, and selenium found in Brazil nuts.
Diagnosing Prostate Cancer
There is no single definite test for prostate cancer. If you suspect you have any of the listed symptoms you should visit your GP. Take along a fresh sample of urine. Your GP will then discuss what should be done next.
- Testing the urine for infection / blood.
- Examine your prostate / digital rectal examination, puts a gloved lubricated finger into your rectum to feel the prostate, may cause discomfort and embarrassment but not painful.
- May do bloods to check for various things but specifically PSA (Prostate Specific Antigen) this will be explained later.
Prostate Specific Antigen (PSA)
It's a protein produced by some of the cells in the prostate gland. It's measured by talking a sample of your blood. It is normal for all men to have a small amount of PSA in their blood.
Changes in PSA levels.
- PSA rises with age on a continuous scale. Infection in urine can cause PSA to rise, hence the need for a urine sample to out rule infection.
- BPH if the gland is larger than normal it will produce more PSA. The exact ratio of size of prostate to PSA level is not known yet.
- Prostatitis - the inflammation of the prostate allows more PSA to leave the gland and enter your blood stream.
- Prostate cancer - this may cause the PSA level to rise however about 15% or one in six men with a normal PSA may have prostate cancer/
- Vigorous exercise e.g. Cycling may affect the PSA. You are advised to refrain from vigorous exercise in the 48 hours prior to getting your blood tested.
- Ejaculation - may affect your PSA level, refrain from sexual activity for 48 hours prior.
- As already discussed having a Digital Rectal Examination (DRE) straight before a PSA test may affect the result.
- Biopsy - If you had a biopsy in the six weeks before the PSA test this can also affect the test.
- If on the Digital Rectal Examination (DRE), the result shows that the prostate gland is enlarged, this could suggest Benign Prostate Hypoplasia (BPH).
- A prostate gland with hard bumpy areas may suggest prostate cancer, in the latter case you will be referred to a specialist (Urologist).
Hospital Tests
If the Digital Rectal Examination (DRE) is suspicious you may have the following tests in hospital.
Transrectal Ultrasound (TRUS) - Guided Prostate Biopsy.
This involves taking 10-12 small samples of tissue from the prostate to be examined under a microscope, at the same time a Transrectal Ultrasound is done which helps the specialist to guide the biopsy needles and measure the size of the prostate gland.
Other ways of taking a biopsy are during a cystoscopy (tube into the bladder) or through the skin behind the testicles (perineum).
Note:- Transrectal Ultrasound (TRUS) guided biopsy can miss up to one in five cancers, because the location of the cancer is unknown. You may need a further biopsy if your symptoms persist or your PSA level continues to rise.
You may receive an MRI Scan if cancerous cells are found, therefore they can be studied further to see how quickly the cancer will spread during the process known as staging or grading.
Depending on the results you may go onto further treatment or they may suggest a wait and see approach keeping an eye on your PSA.
Treatments vary depending on what stage your cancer is at, they will be discussed fully by your consultant.
Remember always bring a fresh sample of urine; it can out rule infection and may help to detect kidney disease, bladder disease and may also pick up diabetes.
Dr. E. J. S. Burke
Provincial Grand Physician
References
PSA and Beyond, published by the Prostate Cancer Charity - copies available at your GP or go to www.prostate-cancer.org Telephone No: 020 8222 7622
Prostate Cancer Risk Management Programme. www.cancerscreening.nhs.uk/prostate